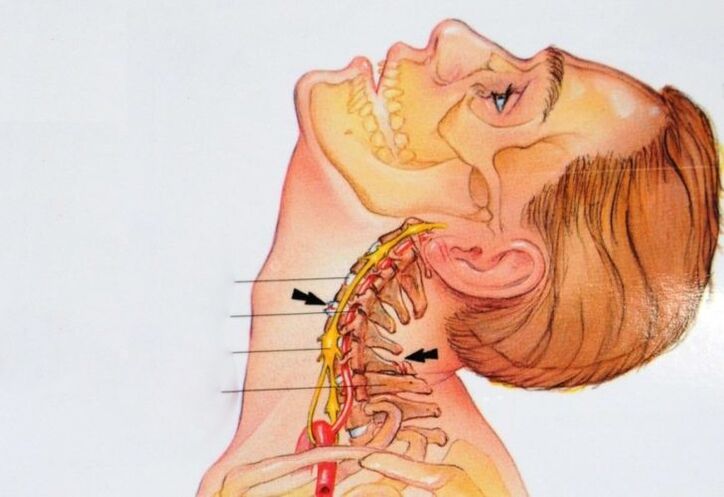
Osteochondrosis of the cervical spine is a disease characterized by damage to the intervertebral discs.
Cervical osteochondrosis is one of the most common diseases in the world. Statistically, about 60% of the world's population faced it, since modern people suffer from physical inactivity, and also spend a huge amount of time in sedentary work. Osteochondrosis manifests itself in the form of damage to the intervertebral cartilage, as well as reactive processes in adjacent tissues.
The vertebrae of the cervical spine are much smaller than the vertebrae of other spine, but the load on them is not less. We constantly turn our heads, which is why the neck is in a systematic movement. At the initial stages, the disease is difficult to recognize, and the basic manifestations of the disease are often ignored by patients. The result is the launch of cervical collar osteochondrosis, which significantly complicates the further process of treatment.
A modern clinic successfully treats osteochondrosis of the neck with non-surgical methods using correction and kinesiotherapy.

Causes of osteochondrosis of the neck
There are several factors that can contribute to the development of osteochondrosis:
- Physical inactivity is the main reason that precedes the development of a dangerous disease. The complete absence of moderate physical activity leads to the degradation of the muscular and bone skeleton. Insufficient daily activity is not only a problem for office workers and drivers. People who prefer to while away their free time at the computer or watching TV suffer from hypodynamia.
- Excessive physical activity. Most often, professional athletes who are exposed to axial loads on the back suffer from this. Work at the limit of possibilities also threatens novice athletes who train without the supervision of a professional trainer and perform exercises with incorrectly set technique.
- Negative factors for posture are walking in high heels and in uncomfortable shoes, scoliosis, flat feet, as well as improper body position during sleep.
- Excess weight puts an excessive load on the spine, leading to displacement of the vertebrae and wear of the cartilaginous structures.
- Rheumatism.
- Disorders of the endocrine system.
- Stress.
- Hypothermia of the neck.
- A sedentary lifestyle (such as drivers and office workers) or excessive physical activity (such as athletes).
As a rule, under the influence of these factors, a load on the cervical vertebrae occurs, which causes the formation of muscle spasm. As a result, the blood circulation process is disrupted and the metabolism worsens, which leads to degenerative changes.
An interesting fact: the risk of developing such an ailment as osteochondrosis is largely associated with evolutionary changes in the human body. It's about walking upright. During the entire life cycle, the spinal column performs the function of the "core" of our body. The vertebrae, pressing on the cartilaginous discs, gradually wear them out, so the connective tissue degrades. Because of this, osteochondrosis often makes itself felt in old age.
Symptoms and treatment of osteochondrosis of the cervical spine will largely depend on the reasons that provoked the onset of the disease. In order to develop an individual therapeutic plan, doctors conduct a whole range of examinations. Self-medication for neck pain is strongly discouraged. Incorrect massages, medicines or traditional medicine methods can aggravate the situation and lead to a host of irreparable consequences!

Cervical osteochondrosis: symptoms and treatment
The manifestations of a dangerous disease depend on 2 main factors:
- Type of load on the cervical spine.
- The site of damage to the cartilaginous structure of the intervertebral disc.
The nerve roots perform a large number of functions, therefore, the symptoms of damage to their individual parts can vary greatly. Additionally, you need to take into account the stage of development of the disease. There are 4 of them, each subsequent of which is heavier than the previous one.
Cervical osteochondrosis 1 degree
This degree is called preclinical and is poorly expressed, which is why patients attribute symptoms to stress, lack of sleep and other seemingly frivolous problems. The spine begins to defend itself against "destructive" movements and excessive stress, so people begin to feel discomfort.
The main symptoms are:
- headache
- discomfort in the neck, shoulders and arms
- mild visual impairment
- a slight decrease in motor activity of the neck
One of the most noticeable symptoms of the preclinical stage of cervical osteochondrosis is the constant tension of the neck muscles. The muscles quickly overwork, which leads to a feeling of bearable pain, as well as a crunch when turning / tilting the head.
Since the above problems do not cause much discomfort, most patients prefer to let the situation take its course. In fact, it is already necessary to begin treatment of osteochondrosis of the cervical spine, because the earlier therapy begins, the more effective it will be.
Cervical osteochondrosis of the 2nd degree
In this case, patients begin to feel perceptible pain when tilting / turning their head. Often, uncomfortable sensations spread to the arms, shoulder joints and hands. Problems with the state of the nervous system begin to appear: a person becomes irritable, absent-minded, his daily working capacity is noticeably reduced. The basic symptoms of cervical osteochondrosis in women are almost identical to the symptoms of problems with the reproductive system (weakness, fatigue, apathetic mood, and much more).
Despite the obvious signs of the development of the disease, it is still possible to get rid of osteochondrosis of the neck. First of all, doctors work to eliminate the risk of hernias, which lead to impaired mobility of the limbs and blood supply to the brain.
The main symptoms are:
- severe neck pain
- noise in ears
- visual impairment
- decreased sensitivity of the skin of the shoulders and arms
- deterioration of tendon reflexes
Cervical osteochondrosis 3 degrees
At this stage of development, the disease is already considered neglected. Treatment of stage 3 cervical osteochondrosis is more difficult, since the destruction / deformation of the cartilaginous structures is often irreversible. The pain syndrome is becoming stronger, which is associated with the active development of hernias and the friction of the bone tissues of the vertebrae against each other.
In addition to pain, the patient experiences weakness and complains of dizziness. The reason for this is the infringement of large vessels and nerves passing through the spine. The brain receives inadequate amounts of nutrition and oxygen, which can lead to clouding of consciousness. The pain radiates to the upper extremities, there is a feeling of weakness in the arms. Another clear sign of grade 3 osteochondrosis is loss of sensitivity in the fingers, as well as tingling in them.
The main symptoms are:
- increased pain
- hernia of the cervical spine
- very weak tendon reflexes
- paralysis of the upper limbs
Cervical osteochondrosis grade 4
The cartilaginous tissues of the intervertebral discs have already undergone major changes due to destruction. At the 4th stage of the disease, in 99% of cases there are protrusions and hernias, which have a significant negative effect on the patient's condition. The body begins independent recovery and "builds up" tissue in the areas of disc damage. As a result, the pillar itself loses its mobility.
As the nerves and blood vessels are compressed, the person loses coordination of movements. Drowsiness, apathy and pain only intensify. Patients often complain of annoying tinnitus. In addition, stage 4 of cervical osteochondrosis threatens a number of the following consequences:
- Cerebral ischemia, the risk of developing spinal stroke. This is due to strong compression of the vertebral arteries.
- Impaired perception of the surrounding world and systematic loss of consciousness. The reason is the pinching of the blood vessels and insufficient blood supply to the cerebral cortex.
- Fatal outcome. A disastrous consequence can arise as a result of spinal cord clamping.
The main symptoms are:
- depression of brain activity
- lack of coordination
- increased dizziness
- paralysis
- hearing and vision loss
- angina pectoris, shortness of breath
How to cure cervical osteochondrosis: the diagnostic stage
Before starting to eliminate the disease, doctors conduct a comprehensive examination of the patient's cervical spine. This is necessary to establish the fact of the presence and neglect of the disease. Diagnostics consists of several stages:
- X-ray. This is a visual way to determine the location of the vertebrae, as well as changes in their mobility.
- Laboratory research. With the help of tests, doctors establish disorders of the spinal column, and also make a final diagnosis.
- CT. This is a modern technique for assessing ruptures and changes in the height of intervertebral discs. Also, computed tomography helps to track the instability of individual vertebrae.
- MRI. The presented stage of the examination is carried out in order to determine the state of the nerve roots, the quality of blood circulation, as well as pathological changes in the cartilaginous / bone structures.
- Differential diagnostics. This includes an ultrasound scan, a cardiogram, and several other procedures. They are necessary in order not to confuse osteochondrosis with other diseases that have identical symptoms. These include diseases of the urinary system, all kinds of deformities of the spinal column, hip injuries, as well as disorders of the central nervous system.
Determination of symptoms and treatment of cervical osteochondrosis is impossible without a comprehensive diagnosis. The sooner it is carried out, the more effective the therapy will be. If you find symptoms of the disease, see your GP as soon as possible. He will give referrals for appointments with specialists of narrower profiles: a neurologist and an orthopedist. In some cases, it may be necessary to consult a cardiologist if signs of the disease overlap with suspected angina pectoris or ischemia of the heart muscle.
In modern clinics, diagnostics and successful treatment of osteochondrosis of the neck are carried out on the basis of the use of kinesiotherapy. With the help of this healing technique, patients, performing a set of physical exercises on special exercise machines for recovery, significantly improve their health.
Treatment of cervical osteochondrosis in women and men basic methods
A high-quality and stable result in the treatment of osteochondrosis of the cervical spine can be achieved only with an integrated approach to the problem. The effectiveness of recovery largely depends on the mood of the patient, who will have to completely revise the lifestyle, diet, sleep and wakefulness.
It is by no means possible to independently treat osteochondrosis of the cervical spine in women and men, since the basic symptoms of the disease can signal the development of a completely different disease. Drugs chosen without the knowledge of the doctor can seriously aggravate the situation. Even an elementary intake of painkillers does not always have the expected effect, which once again proves the need for preliminary consultation with a specialist.
Elimination of exacerbations of pain
The disease often manifests itself in the form of a stabbing, aching and pulling pain syndrome. The main task of the doctor is to alleviate your suffering, therefore, first of all, specialists prescribe:
- Anti-inflammatory drugs;
- Vitamins;
- Pain relievers;
- Chondroprotectors.
The last category of drugs is aimed at restoring cartilaginous structures, which is especially important in advanced stages of the disease. Additionally, patients are prescribed medications to relieve muscle spasms and improve blood flow in the body.
Therapeutic gymnastic exercises
Specialists in physical therapy know how to get rid of cervical osteochondrosis in the most affordable ways. Exercise therapy is one of the most effective methods of treating osteochondrosis, which can be used even at home. The intensity of the exercise in this case does not play any role. The regularity of moderate physical activity will help to achieve the result. Here's the effect of exercise:
- Strengthening the muscles in the neck, which are responsible for supporting weakened vertebrae.
- Stimulation and normalization of blood supply in the body, which is especially important for the cerebral cortex.
- Increase of the general tone, charge of energy, restoration of productivity and work capacity of a person.
Exercise therapy classes are allowed on a daily basis. The set of exercises includes all kinds of head rotations and tilts. With the proper level of physical fitness, the level of difficulty increases and hand movements are connected to work. The advantage of therapeutic gymnastic elements is that they can be used even in the workplace. But remember that they can be performed only after the acute pain syndrome has been eliminated.
As an additional load, doctors recommend that patients visit the pool, since swimming relieves stress on the spine and relieves stress from the intervertebral discs. Shown and work with light dumbbells in order to strengthen the shoulder girdle.
Physiotherapy
Physiotherapy methods are numerous:
- Electrophoresis.
- Magneto, laser, and shock wave therapy.
- Mud therapy.
- Medicinal baths and showers.
The above are only the main therapeutic methods that are aimed at restoring the blood supply to the affected spinal column, eliminating inflammation, pain, and slowing down the process of neck ossification.
Massage
Treatment of cervical osteochondrosis of the spine with massages is widespread throughout the world. But this method must be used with great care, since a rough and inept impact on the damaged parts of the neck can lead to a worsening of the condition. Before making an appointment with a masseur, you should consult with your doctor.
Thanks to the influence of the hands on the sore area, muscle tone decreases, which leads to getting rid of painful spasms. It also improves blood circulation, restores clarity of thought and general well-being of the patient.
Surgery
The last stage of the development of the disease leads to the formation of serious intervertebral hernias, as well as a narrowing of the lumen of the spine. Treatment of the patient in this case may require surgical intervention. The surgeon decides whether an operation is necessary. He also determines the complex of preparatory measures, the period of postoperative recovery and rehabilitation.
Most surgical interventions involve the removal of the resulting hernias, as well as the replacement of damaged vertebrae.
Treatment of cervical osteochondrosis in the clinic
Treatment of osteochondrosis of the cervical spine in a professional clinic involves the use of exclusively non-surgical methods. Specialists work according to a unique technique developed on the basis of the principles of kinesiotherapy. Patients who turn to us for help are treated with a set of physical exercises in a specially equipped room.
Treatment of cervical osteochondrosis takes place according to an individually developed program. The therapeutic effect is not only on a specific part of the spinal column, but also on the internal organs. The drug-free and non-surgical treatment process is difficult, but we provide comprehensive support to patients, help them become more decisive and reconsider their attitude towards their own illness.
This is what the healing process is built from:
- Trainings in the rehabilitation room at least 2-3 times a week.
- Parterre therapeutic gymnastics.
- Thermotherapy according to individual indications.
- Pain relief with ice massage.
- Therapeutic / restorative massage.
- Adaptive exercises for work at home.
- Micro-anatomical studies of ultrasound in order to track recovery over time.
- Personal consultations with the specialists of the kinesitherapy clinic.

Prevention of osteochondrosis
Treatment of osteochondrosis of the cervical spine in the context of modern medicine includes many effective methods. But it is much better not to allow this problem to appear at all than to deal with its elimination. There is a set of preventive measures that will minimize the risk of the appearance and development of a dangerous ailment:
- Take a 10-minute hot shower daily. A systematic visit to the baths / saunas is also recommended. Please note that these recommendations are only suitable for people with no cardiovascular health problems.
- Go swimming and take regular walks in the fresh air at a relaxed pace. Physical inactivity is one of the main causes of diseases of the musculoskeletal system.
- Refuse excessive physical exertion at the limit of human capabilities. This is especially true when working in gyms. Critical axial loads on the spine lead to protrusion.
- Try to avoid back stabs, especially if you are over 30 years of age.
- Review your diet. Try to exclude confectionery, flour, moderate salt and sugar intake. Reducing the calorie content of foods allows you to avoid gaining excess weight, which puts additional stress on the spinal column.
- If you work in an office and spend a lot of time at the computer, take care of purchasing a special chair with lumbar and neck support. Try to do basic warm-up exercises every 60 minutes.
- In the event that pain appears after waking up, consider buying an orthopedic mattress and pillow. If possible, get a bed with a flat, hard surface.
- To avoid degenerative and dystrophic changes in the cervical spine, visit a professional massage therapist at least 2-3 times a year. Neck and collar massage is one of the most effective preventive measures.
- Women should minimize walking on high-heeled shoes, as this interferes with the natural position of the spine. With diagnosed flat feet, it is recommended to buy special shoes or insoles, since orthopedic products correct the position of the foot and relieve unnecessary stress from the spinal column.
As well as:
- you should visit the bath regularly
- you need to give up bodybuilding, which can contribute to the protrusion of the cervical disc
- gentle exercise can be a good prevention of disease
Outcome
Treatment of osteochondrosis in a professional clinic takes place under the strict supervision of highly qualified specialists. Doctors adhere to an integrated approach in working with patients and even deal with advanced stages of the disease. If you notice symptoms of osteochondrosis, you do not need to endure, self-medicate and delay a visit to the doctor. Start your journey to a healthy, happy life!
















































