
There is practically no person who at least once in his life would not experience back pain in the lumbar region. This is how we pay for upright walking and our everyday habits.
In addition to damage that can affect the spine, its muscles, nerves and ligaments, it should be borne in mind that sometimes the back hurts in the lumbar region with internal diseases - diseases of the kidneys, gastrointestinal tract, and female genital organs.
Symptoms of low back pain can range from dull to sharp. The pain may go away on its own or become chronic (the symptom has been present for more than three months).

Dangerous! You should immediately consult a doctor if:
- pain in the lumbar region arose abruptly after an obvious back injury;
- the temperature has risen sharply, there are vegetative disorders, loss of consciousness, sweating, difficulty breathing;
- involuntary emptying of the intestines and bladder occurs;
- there is numbness in the groin area;
- there was weakness of the lower extremities, their paresis or paralysis, impaired sensitivity;
- pains are given to the stomach and sharply increase when coughing or sneezing;
- symptoms appeared against the background of a sharp weight loss, prolonged use of steroids, immunodeficiency;
- in the family history there were cases of cancer, inflammatory or degenerative diseases of the bone and cartilage tissue.
Why does the back hurt in the lumbar region?
Myofascial pain
A muscle strain or spasm can develop gradually or happen suddenly. With a high load, damage affects not only muscle fibers, but also the ligamentous apparatus and fascia.
Muscular pain in the lower back appear after:
- lifting heavy weights or overexerting yourself at work or playing sports;
- playing sports from time to time. Muscles are especially vulnerable if you are inactive during the work week and then spend hours in the gym on weekends;
- a sharp increase in the weight of one's own body, behind which muscles do not have time to grow;
- prolonged sitting or standing in an uncomfortable position;
- everyday carrying of a bag in one of the hands or over the shoulder;
- posture disorders. The spine performs its best supportive and protective function when you are not slouching. The muscles in the lower back experience the least stress when you sit with good support under your lower back, and in a standing position, evenly distribute the weight on both legs.
If the back hurts after a bruise, fracture, sprain, hypothermia, an infectious disease or an established helminthic invasion, then myositis (inflammation) of the muscles of the lower back can be suspected. Severe pain is constantly present due to inflammation of the muscle fibers, "nodules" are felt in the muscles - places of spasm. Inflammation can be acute or take a chronic form. With a long course of the disease, the pain is unstable, aggravated by prolonged lying or sitting, in the late afternoon or when the weather changes. Touching the muscles causes a feeling of soreness and discomfort, the muscles of the lower back are in constant tension, inflammatory edema is formed, the temperature rises locally and at the level of the whole organism.
With muscle spasm, the roots of the spinal nerves are infringed, so attacks often resemble a picture of sciatica or sciatica - there are burning severe pains along the back of the thigh and lower leg, the limbs become numb, they lose sensitivity. The pronounced muscle tone in myositis makes the patient take a forced position, he walks and lies hunched over, moves on bent legs.
How to treat muscular pain of the spine? Non-steroidal anti-inflammatory drugs and analgesics are used to eliminate inflammation and pain. Medicines can be taken in the form of tablets, ointments, injections, transdermal patches with a gradual release of active substances. Irritating and warming ointments are also used, which reflexively increase blood flow to the muscles of the lower back. A larger volume of inflowing blood contributes to the washing out of the products of inflammation and tissue breakdown.
The reduction of inflammatory edema is facilitated by injections of corticosteroids and vasoconstrictive drugs.
If the cause of myositis is an infection or poisoning of the body with worm toxins, then initially antibiotics or anthelmintic drugs are used. In this case, warming ointments or compresses cannot be used.
Spinal diseases involving nerve endings
In the lumbar region, the vertebrae are separated by elastic cartilaginous discs, which protect the spine from injury, but are themselves subject to wear and aging.
Normally, the disc is a jelly-like nucleus pulposus surrounded by a denser layer of the annulus fibrosus. The elasticity of the core is due to its ability to bind and retain water: when the load increases, it accumulates water, and elasticity increases, when the pressure decreases, the core releases water and becomes flatter.
Osteochondrosis in the vertebral region develops when the intervertebral discs are malnourished (their "drying out") or with excessive local load. Most often, lower back pain is due to the fact that the lower poles of its intervertebral discs bear the greatest load when sitting, when lifting weights in front of them. At the same time, tears, displacements form in the discs, the vertebral ligaments are damaged, there is a constant aching pain, pulsation.
Pain in the spine has several mechanisms of development:
- violation of microcirculation in the tissues surrounding the spine and, in particular, in the spinal canal, the formation of congestion and edema. Such conditions develop against the background of hypothermia, overheating, inflammatory processes.
- degenerative processes in the fixing ligaments of the spine. An increase in the mobility of the vertebrae leads to their slight displacement and non-physiological compression, which causes infringement of nerves, blood vessels, and the formation of hernias.
- axial compression of the vertebrae when lifting weights or damage to them during excessive rotation (turn).
- aseptic inflammation. The destruction of the nucleus leads to the release of sensitizing factors into the spinal canal. There is irritation of the nerve endings, which causes a spasm of the muscles that infringe on the neighboring vertebrae - above and below the hernia. Gradually, the reaction covers the entire lumbar region and leads to the fact that any movement causes a sensation of pain.
A weakened disc can rupture, resulting in a bulge, protrusion, or prolapse of the nucleus, and eventually a herniation. The appearance of a hernia puts pressure on the spinal cord and spinal nerve roots. In such conditions, a throbbing pain in the lower back appears sharply, which diverges along the path of the pinched nerve. The most well-known cases of compression of the sciatic nerve (sciatica), which are manifested by sharp pain along the back of the thigh and lower leg, numbness of the limb from the side of the hernia, muscle weakness, involuntary twisting of the legs.
Pain in the lumbar spine is aggravated when sitting and standing, when turning, bending over. Often there is a protective muscle reaction - a painful contraction of the muscles (formation of rollers) on both sides of the spine, which isolates the department from unnecessary movement. Osteochondrosis subsequently leads to the appearance of sciatica (inflammation of the roots of the spinal nerves).
The radicular syndrome is dangerous when the nerves of the lower back, which are responsible for the innervation of the internal organs (horns of the cauda equina), are pinched. At the same time, pain is given to the stomach, the function of the bladder and intestines is disturbed, there are problems with potency in men and gynecological diseases in women.
Many patients, due to the fact that the lower back hurts very much, take analgesic postures - they deviate the body to the left, if the right side hurts, lie on the right side. If the hernia is on the left. Also characteristic is the appearance of severe pain when pressing on a hernia in the intervertebral space (ringing symptom).
How to treat if your back hurts with osteochondrosis:
- during an attack of pain, you can take an anesthetic pose - lie on your back, and put a roller under your knees. It is also recommended to sleep on a hard surface;
- from analgesic drugs, NSAIDs can be taken orally or as injections on both sides of the spine in the lumbar hotel;
- use local irritants as a distraction therapy - mustard plasters, iodine mesh, pepper patch and ointments;
- eliminate myotic spasm through manual therapy, acupuncture, vacuum massage, reflexology, gymnastics;
- during the attenuation of the acute period, mud treatment, ozocerite, warming up can be used.
Treatment of pain in radicular syndrome includes:
- providing bed rest, lumbar traction (dry or underwater);
- the use of novocaine blockades at the site of infringement, the use of NSAIDs or weak opiates;
- physiotherapy - microcurrent stimulation, electrophoresis with analgesics.
Indications for surgery are constant acute pain, as well as impaired function of internal organs, development of paralysis of the limbs, sequestration of a hernia in the spinal canal.
Degenerative inflammatory lesions
Spondylarthrosis (inflammation of the facet joints of the vertebrae) occurs with degeneration, a decrease in the height and volume of the intervertebral discs. Pain in the lower back appear from overstretching the capsule and increasing pressure on the surface of the intervertebral joints. Pain causes the patient to bend more in the lower back, thus increasing the overload of the intervertebral joints. Especially discomfort in the lower back is aggravated by wearing shoes with heels, walking for a long time, descending from elephants, positions when the body deviates backwards, for example, when looking at something above the head.
In patients with this diagnosis, stiffness in the lower back is noted in the morning, the pain increases during the day or after exercise. It has a diffuse character and it is difficult to clearly show the boundaries: discomfort is determined in the gluteal muscles, inguinal region, lower abdomen, and in the scrotum in men. This spondyloarthrosis differs from radicular syndrome, when you can pinpoint the source of pain.
What to do to relieve pain? It usually helps to take a supine position, bending the legs at the hip and knee joints.
Their drugs are preferred non-steroidal anti-inflammatory drugs and non-narcotic analgesics.
Muscle relaxants are also added as they relieve muscle tension and improve spinal mobility.
Psychotherapy has a positive effect, since chronic pain introduces the patient into a state of depression.
Spondylosis, unlike osteochondrosis, affects the fibrous ring of the intervertebral disc and the anterior longitudinal ligaments more. With this disease, calcification of connective tissue structures occurs with the formation of growths along the edge of the vertebrae - osteophytes. These formations cause a violation of microcirculation near the nerve roots and lead to the fact that the back hurts in the lower back, and the mobility of this department is also limited.
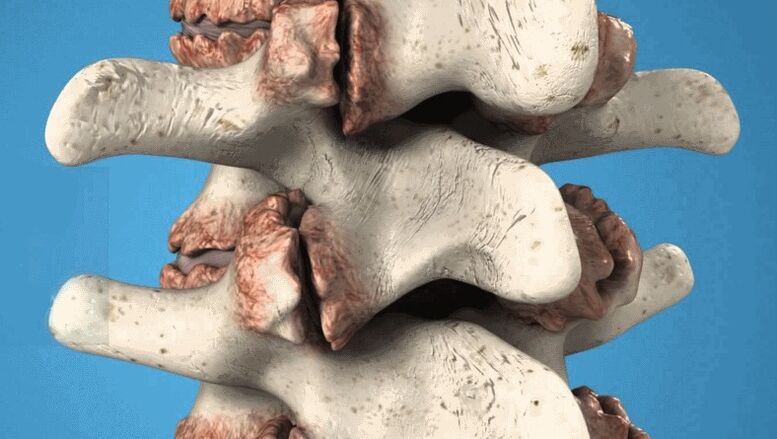
Vertebral osteophytes are pathological growths that damage nerves and blood vessels.
Treatment is usually conservative, with the use of anti-inflammatory drugs, analgesics, vitamins. A good effect is given by electrophoresis with novocaine, lidase, manual therapy, physiotherapy (amplipulse, laser installation, shock wave therapy to destroy compacted elements and increase spinal mobility).
Note! In the advanced stage, osteophytes do not resolve. While their size is small, the treatment is aimed at eliminating inflammation, pain, improving metabolism. If the back does not hurt very much, then nothing is done with the growths. If osteophytes cause persistent pain or are large, they can be removed during surgery.
Diseases of a tumor nature
Low back pain can occur from compression of the spinal cord by a tumor from the outside (extramedullary formations) and from the inside (intramedullary, originating from the cerebrospinal substance itself).
Cells of various tissues can grow pathologically:
- fatty - a lipoma is formed;
- nerve roots - neuroma;
- spinal cord vessels - hemangioma;
- auxiliary tissue - glioma;
- bone tissue - osteosarcoma;
- cartilage - chondrosarcoma.
The tumor process, especially malignant, is characterized by a pain syndrome that resembles sciatica (it can be unilateral and bilateral), a general deterioration in the patient's condition, and exhaustion.

If the pathology affects the area of I-IV lumbar vertebrae, then there is a burning pain in front and on the sides of the upper thigh, incomplete paralysis of this area.
With a lesion in the region of the IV lumbar - II sacral segments, numbness of the paragenital region, impaired motor and sensory innervation of the gluteal muscles, posterior thigh, calf, fecal and urinary incontinence are noted.
A pronounced disturbance in the functioning of the pelvic organs occurs with a neoplasm in the region of the V-III sacral vertebrae. The patient suffers from sexual impotence or menstrual disorders, constipation or fecal and urinary incontinence.
Treatment of tumors is specific, painkillers, and anticancer drugs are prescription drugs.
As you can see, low back pain is usually caused by musculoskeletal pathologies. They can be diagnosed by clinical signs and research data, the main task of which is to correctly determine the nature of the disease and not confuse it with oncological causes, diseases of internal organs or trauma. If you experience lower back pain, we recommend that you always seek the advice of a neurologist or orthopedist.
















































